Heart Failure: A Modern Scientific Perspective, Diagnosis, and Treatment
- Health Communicator

- Jun 22
- 4 min read
Updated: Sep 3
AUDIO:
Overview
Heart failure (HF) is a complex clinical condition in which the heart is unable to pump enough blood to meet the body’s needs. This insufficiency results from structural or functional impairments that affect the heart’s ability to contract and relax properly.
There are two main types of HF:
Heart Failure with Reduced Ejection Fraction (HFrEF): when the heart’s left ventricle pumps out less than 40% of the blood it contains.
Heart Failure with Preserved Ejection Fraction (HFpEF): when the heart’s pumping ability is relatively preserved, but it cannot relax and fill effectively.
Heart failure is a chronic, progressive condition. Its incidence increases with age and is especially common in developed countries. In the United States, approximately 6.7 million people are living with heart failure, and that number is expected to rise significantly in the coming years.

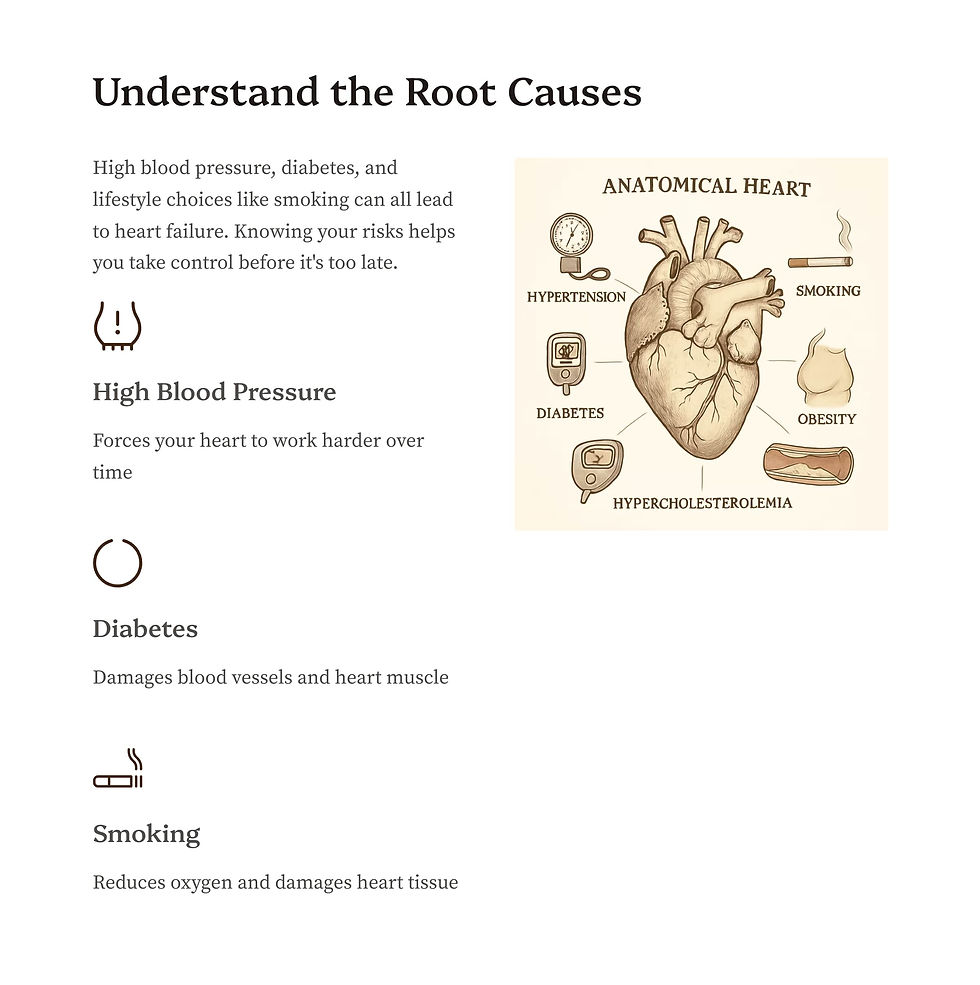


Causes and Risk Factors Heart failure can arise from various causes and contributing factors:
High blood pressure (hypertension): Long-standing high blood pressure leads to thickening of the heart muscle and eventually to fatigue and dysfunction.
Coronary artery disease: After a heart attack, scar tissue can form in the damaged heart muscle, reducing the heart’s ability to pump efficiently.
Obesity and metabolic syndrome: These conditions increase cardiac workload, promote inflammation, and accelerate heart damage.
Diabetes mellitus: Increases HF risk by damaging small blood vessels and having toxic effects on heart muscle cells.
Genetic predispositions: Certain types of cardiomyopathies and specific genes increase the risk, particularly in families with a history of heart disease.
Unhealthy lifestyle habits: Smoking, excessive alcohol use, and physical inactivity significantly raise the risk of heart disease.
Other contributing factors: Age, chronic kidney disease, certain medications, and socioeconomic conditions.
Example: In younger individuals, leading risk factors include obesity and high blood pressure, while in older adults, the cumulative effect of coronary artery disease and diabetes is more prominent.
Key Symptoms Heart failure symptoms stem from reduced oxygen delivery to tissues and fluid retention:
Shortness of breath (dyspnea): Initially occurs with physical activity, later even at rest. It may also appear at night when lying flat (orthopnea).
Fatigue and weakness: Often overlooked early on but become more noticeable as the condition worsens.
Swelling (edema): Especially in the ankles, legs, and abdomen, due to fluid buildup.
Frequent nighttime urination (nocturia).
Abdominal discomfort or heaviness: Due to liver congestion.
These symptoms often worsen over time and help define the severity of the disease.
Diagnosis (Expert Opinions) Diagnosing heart failure requires a comprehensive approach:
Medical history and physical exam: The doctor will ask about symptoms and risk factors and look for signs like swelling, neck vein distension, and others.
Biomarkers: Blood levels of BNP and NT-proBNP rise in response to stress on the heart muscle and are particularly useful in diagnosing and monitoring HF.
Echocardiography: This ultrasound exam is the primary tool for evaluating heart function, measuring ejection fraction, and identifying structural abnormalities.
Additional testing: Coronary angiography is used if coronary artery disease is suspected; cardiac MRI may be used in more complex cases.
Expert insight: Combining clinical symptoms, biomarkers, and imaging improves diagnostic accuracy and helps tailor treatment to individual needs.
Treatment and Guidelines (Official Recommendations) Modern management includes a mix of medications, lifestyle changes, and, when needed, device-based therapies:
HFrEF (reduced ejection fraction):
ACE inhibitors/ARBs/ARNIs: Block harmful hormonal responses, reduce mortality.
Beta-blockers: Improve survival and reduce the risk of recurrent hospitalizations.
Mineralocorticoid receptor antagonists (e.g., spironolactone, eplerenone): Especially effective in more severe cases.
SGLT2 inhibitors (e.g., dapagliflozin, empagliflozin): A newer class of medications proven to reduce hospitalizations and death, even in people without diabetes.
HFpEF (preserved ejection fraction):
The main focus is symptom control and managing associated conditions (hypertension, diabetes, obesity).
Diuretics are used to reduce fluid overload.
Devices:
Implantable defibrillators and cardiac resynchronization therapy are recommended for certain high-risk patients.
Non-pharmacological therapy:
Medically supervised physical activity (cardiac rehab), salt restriction, weight loss, and quitting smoking.
Management of blood pressure, blood sugar, and cholesterol levels.
Acute cases: When symptoms worsen, rapid intervention with diuretics and adjustment of therapy is essential, depending on the individual’s condition and coexisting illnesses.
Latest Scientific Advancements
SGLT2 inhibitors have revolutionized heart failure treatment, showing clear benefits even in HFpEF.
Finerenone, a newer mineralocorticoid receptor antagonist, is being studied for safety and effectiveness in patients with decompensated HF and preserved ejection fraction.
Digital tools and telemonitoring (e.g., SmartHF) enable real-time treatment adjustments and help patients adhere to their care plans.
Personalized medicine: More extensive use of cardiac MRI, biomarkers, and genetic testing allows for more precise diagnoses and individualized therapies.
Emerging drugs like vericiguat and omecamtiv mecarbil show promise for high-risk patients but are still under investigation.
Expert Consensus Key takeaways from leading specialists and medical societies:
Early diagnosis and timely treatment greatly improve survival and quality of life.
Rapid initiation of comprehensive medication therapy is especially important for HFrEF.
Lifestyle changes—including weight management, physical activity, salt restriction, and eliminating harmful habits—are essential parts of treatment.
For HFpEF, more research is needed to identify effective treatments, but symptom control and risk factor management are the current focus.
Personalized approaches, including digital health tools and genetic testing, are expected to play a central role in the future of heart failure care.
Conclusion
Heart failure is a significant public health issue with multiple contributing factors. It requires an integrated, personalized approach to care. Early diagnosis, an optimal combination of drug and non-drug therapies, and strict control of associated risk factors are critical for improving prognosis and quality of life. Ongoing scientific progress—particularly in digital health, personalized medicine, and innovative drug development—opens up new opportunities for increasingly precise and effective management of this complex condition.
Key References:
Universal Definition and Classification of Heart Failure. Bozkurt et al., European Journal of Heart Failure (2021). https://doi.org/10.1002/ejhf.2115
Heart Failure With Reduced Ejection Fraction: A Review. Murphy et al., JAMA (2020). https://doi.org/10.1001/jama.2020.10262
Heart Failure With Preserved Ejection Fraction: A Review. Redfield & Borlaug, JAMA (2023). https://doi.org/10.1001/jama.2023.2020
2024 Heart Disease and Stroke Statistics: A Report of US and Global Data From the American Heart Association. Martin et al., Circulation (2024). https://doi.org/10.1161/cir.0000000000001209
Hypertension and Heart Failure: Prevention, Targets, and Treatment. Di Palo & Barone, Heart Failure Clinics (2020). https://doi.org/10.1016/j.hfc.2019.09.001
Heart Failure: An Underappreciated Complication of Diabetes. Pop-Busui et al., Diabetes Care (2022). https://doi.org/10.2337/dci22-0014
Heart Failure Epidemiology and Outcomes Statistics. Bozkurt et al., Journal of Cardiac Failure (2023). https://doi.org/10.1016/j.cardfail.2023.07.006
2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure. Heidenreich et al., Circulation (2022). https://doi.org/10.1161/CIR.0000000000001063












Comments