Interleukins – The New Language of the Immune System in Inflammatory Bowel Disease
- Health Communicator

- Jun 22
- 5 min read
Updated: Jul 10
The information in this article is based on the latest scientific review “Key Interleukins in Inflammatory Bowel Disease – A Review of Recent Studies,” published in 2025 in the International Journal of Molecular Sciences. The study was led by Professor David Aebisher (Department of Photomedicine and Physical Chemistry, Medical College of The Rzeszów University, Poland). Co-authors of the publication include Dorota Bartusik-Aebisher, Agnieszka Przygórzewska, and Paweł Woźnicki (Medical College of The Rzeszów University), as well as Piotr Oleś and Professor Aleksandra Kawczyk-Krupka (Medical University of Silesia in Katowice, Poland). The authors are leading researchers, educators, and physicians specializing in molecular medicine, biochemistry, internal medicine, and clinical diagnostics. This review presents the most recent findings on the mechanisms behind inflammatory bowel disease (ulcerative colitis and Crohn’s disease) and the role of key immune mediators—interleukins—in the development, diagnosis, and treatment of these conditions. The questions and answers below are based entirely on the data summarized and analyzed by this respected team of experts.
“Interleukins not only trigger but may also ‘lock down’ inflammation in the gut—understanding them is key to better treatment and renewed hope for patients.”


Expert Insights
Inflammatory Bowel Diseases (IBD)—primarily ulcerative colitis and Crohn’s disease—are serious, chronic immune disorders of the gastrointestinal tract. Their pathogenesis is complex and multifactorial, involving interactions between genetic predisposition, environmental factors, gut microbiota, and particularly, key immune mediators such as interleukins. With the rising incidence of IBD worldwide and the significant side effects and limitations of current therapies, the latest scientific discoveries and expert medical opinions are critically important for patients and their families. Below you’ll find five key expert perspectives and quotes, along with questions and explanations that may help patients better understand their treatment options and current scientific trends.
1. What are the latest scientific findings on the role of interleukin-1β (IL-1β) in IBD?
“Shaul et al. Canakinumab used in children with a very early form of inflammatory bowel disease with an autoinflammatory phenotype resulted in significant improvements in clinical symptoms and biochemical markers of the disease, reduced hospitalization rates, and length of hospitalization.” “Cai et al. Molecule 10v blocking IL-1β signaling via the NLRP3 and AIM-2 inflammasome and reducing STAT1 and STAT5 expression in the JAK/STAT pathway achieved better efficacy than sulfasalazine in a mouse model.”
Comment: New therapies targeting IL-1β show promising results in patients—especially children—who don’t respond well to standard treatments. This points to the need for more individualized approaches in adult cases as well.
2. Why is interleukin-6 (IL-6) central to maintaining chronic inflammation in IBD, and are there new therapeutic approaches?
“IL-6 contributes to damage of the intestinal epithelial barrier during inflammation by increasing its permeability through increased expression of claudin-2, a tight junction protein... Trans-signaling is thought to be the reason for the chronic inflammatory effect of IL-6.” “Selective inhibition of IL-6 trans-signaling may provide clinical benefit with fewer side effects than in the case of global IL-6 blockade. Recently, innovative bi-specific cytokine inhibitors have been developed... They block key inflammatory pathways in IBD.”
Patient Tip: If your condition doesn’t respond well to standard therapy, ask your doctor about enrolling in clinical trials for new IL-6 inhibitors.
3. What is the importance of interleukin-10 (IL-10) in immune control of IBD, and what are the therapy prospects?
“An increase in IL-10 levels is therefore desirable in IBD. An increase in IL-10 expression has been successfully achieved in recent studies by, among others, mesenchymal stem cells, microbiota or... pharmacological potassium channel KCa3.1 blockade.” “Currently, after promising results in a mouse model, the AMT-1 molecule (#NCT04583358), which acts by concentrating biologically active IL-10 on the intestinal lamina propria, is in phase 2 clinical trials.”
Explanation: IL-10 suppresses excessive immune responses, and some new therapies aim to boost this natural mechanism. In the future, more treatments based on cellular and molecular modulation may become available.
4. What should we know about innovative biologic drugs targeting IL-12 and IL-23 in IBD?
“Ustekinumab, an IL12/23p40 antagonist, was approved by the Food and Drug Administration for CD treatment in 2016, and clinical data showed that patients experienced symptom relief and achieved clinical remission of IBD.” “The results of these papers are consistent and confirm the beneficial effect of treatment with mirikizumab [IL-23p19 inhibitor] in inducing clinical, endoscopic, and histological remission and improving patients’ quality of life. At the same time, no new significant safety concerns have been raised.”
Patient Tip: If you suffer from Crohn’s disease or ulcerative colitis that doesn't respond to standard treatment, talk to your gastroenterologist about the potential benefits of these new biologics.
5. What are the risks and potential benefits of blocking IL-17 and IL-22 in IBD?
“The effects of anti-IL-17 treatment are disappointing. Both secukinumab and brodalumab showed worse outcomes in Crohn’s patients treated with IL-17 blockade than in the placebo group. A possible reason... is that, in addition to its ability to induce mucosal inflammation, IL-17A may also contribute to the regeneration and repair of the intestinal mucosa after inflammation has subsided.” “The role of IL-22 in IBD is controversial. Most studies have shown that IL-22 plays a protective role in the acute phase... but if IL-22 signaling is not properly controlled, it can also induce malignancy.”
Comment: Not all interleukin inhibitors are equally safe or effective—some may even worsen the condition. Treatment must be carefully personalized and monitored by an experienced specialist.
Questions and Answers
1. What are the main forms of IBD and how do they differ?
Answer: IBD mainly includes two diseases: ulcerative colitis (UC) and Crohn’s disease (CD). Ulcerative colitis primarily affects the colon, spreading upward from the rectum. Inflammation is continuous and usually limited to the mucosal layer. Crohn’s disease can affect any part of the digestive tract—from mouth to anus—with patchy inflammation, meaning both diseased and healthy segments coexist, and the inflammation extends deeper into the bowel wall.
2. What factors contribute to the development of IBD, and why are case numbers increasing?
Answer: IBD development is multifactorial—it involves genetics, environmental triggers like stress, antibiotic use, diet, smoking, sleep disturbances, and hygiene habits. IBD incidence is increasing in both industrialized and developing countries, likely due to changes in lifestyle and environment.
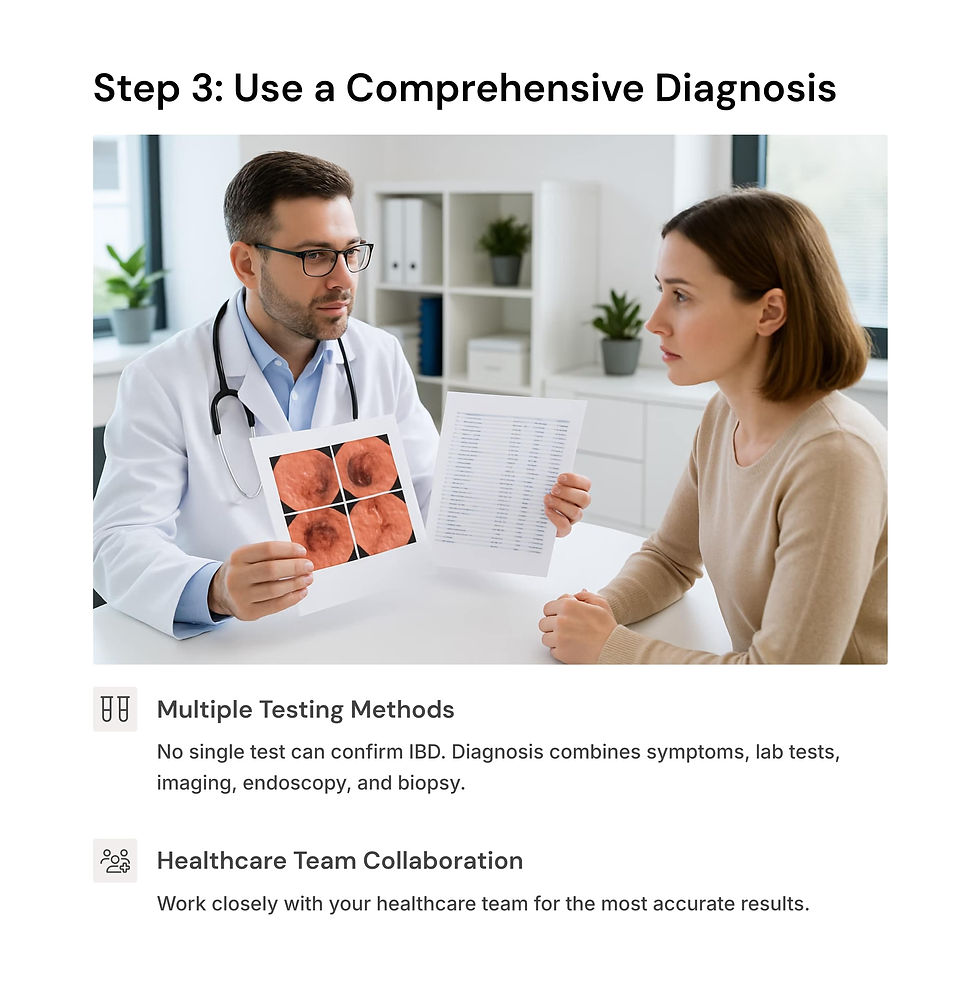
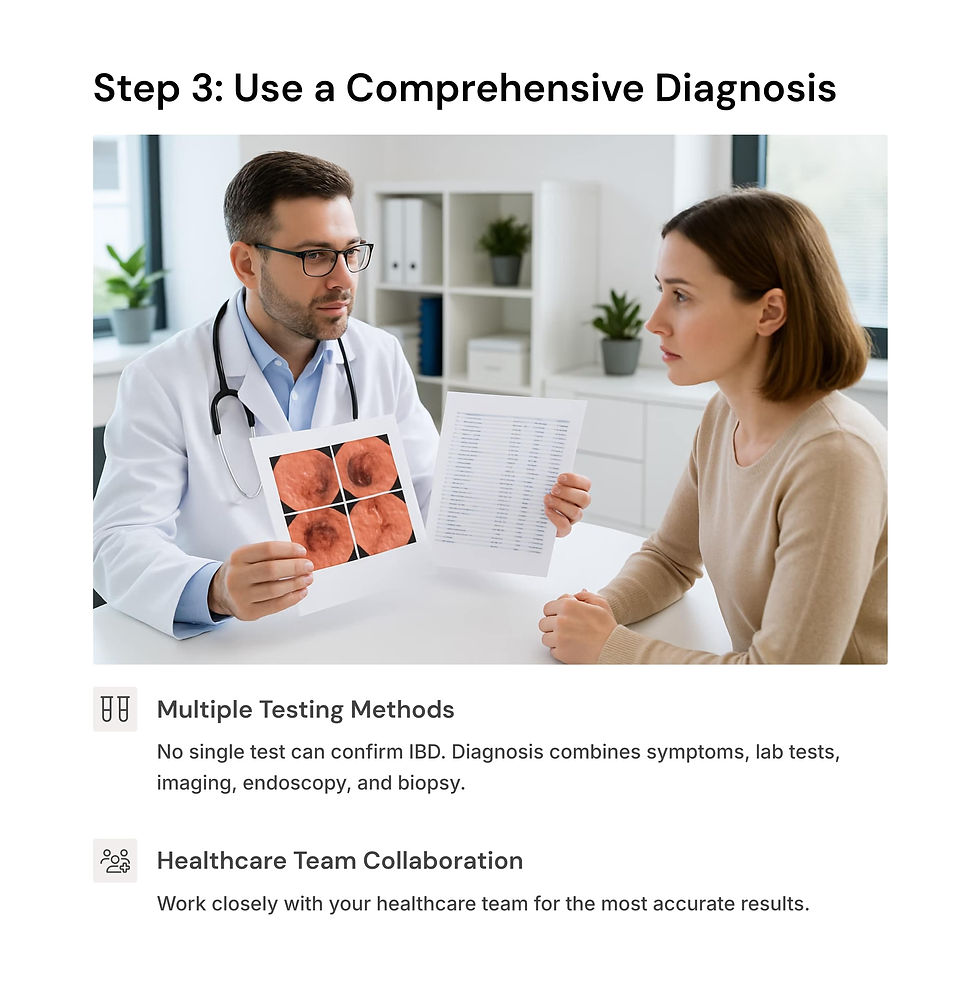
3. How is IBD diagnosed, and why is there no single “gold standard” test?
Answer: IBD diagnosis requires a combination of clinical symptoms, lab tests (e.g., checking for anemia and nutrient deficiencies), imaging (such as ultrasound or CT scans), endoscopy (camera inspection of the gut), and histology (biopsy analysis). There is no single diagnostic marker for IBD, so a comprehensive approach is used.
4. What are the current treatment goals and main strategies for IBD?
Answer: The primary treatment goal is healing of the intestinal lining, as inflammation often continues even after symptoms fade. Strategies include medications such as aminosalicylates, corticosteroids, immunosuppressants, biologics, and new small-molecule drugs that suppress the immune response. Dietary therapy is used as an adjunct, though its effects are usually temporary.
5. What risks and complications should IBD patients consider with standard treatment?
Answer: Many IBD medications can have side effects: aminosalicylates are usually well-tolerated, but sulfasalazine may cause infertility, anemia, and photosensitivity; corticosteroids can lead to infections, high blood pressure, osteoporosis, and more; immunosuppressants and biologics are effective but costly, and some patients either don’t respond or lose response over time. Up to 40% of patients don’t respond to anti-TNF therapy, and up to 46% may lose their response within one year.
Conclusion
In conclusion, the review article by Aebisher et al. provides an exceptionally comprehensive and systematic analysis of the latest scientific discoveries and clinical trends in inflammatory bowel disease. The answers to key questions concerning patients and their families are based entirely on evidence and clinical experience shared by leading European researchers and physicians. The complexity of disease mechanisms, diagnostic challenges, current treatment possibilities and limitations, and the future prospects for individualized molecular-immune-based therapies are clearly outlined. For every IBD patient, being informed, maintaining a critical outlook, and discussing new scientific developments with their physician are essential steps toward effective disease management and improved quality of life.
Source: Aebisher, D.; Bartusik-Aebisher, D.; Przygórzewska, A.; Oleś, P.; Woźnicki, P.; Kawczyk-Krupka, A. "Key Interleukins in Inflammatory Bowel Disease—A Review of Recent Studies." International Journal of Molecular Sciences. 2025, 26, 121. https://doi.org/10.3390/ijms26010121




Comments